Abstract
Introduction:
Skeletal-related events (SREs) can cause significant morbidity and adversely impact quality of life in patients with multiple myeloma (MM). The bisphosphonate zoledronic acid (ZOL) has historically been the most widely used agent to prevent and treat SREs in this population. In 2018, a landmark trial by Raje et al showed that denosumab (DEN), a monoclonal antibody against the receptor activator of nuclear factor-kappa B ligand (RANKL), was non-inferior to ZOL in time to SREs. The use of DEN has since been incorporated into official guidelines and there has been a significant uptake of DEN use in clinical practice, with some patients being switched from ZOL to DEN. Currently, there is a lack of data on the clinical and biological impact of the use of DEN following prior exposure to ZOL in patients with MM. Some have suggested that the use of DEN in patients extensively treated with ZOL may over-suppress bone turnover and recommend the use of bone resorption markers such as C-terminal telopeptide (CTX) to guide this treatment decision. In this observational study, we describe the reasons for the switch in use of these bone-modifying agents (BMAs) and evaluate the incidence of SREs in a selected population of MM patients who received both agents during their course of treatment.
Methods:
This retrospective study included all MM patients that were treated at Yale Cancer Center including Smilow Cancer Hospital and Smilow Care Centers between January 1, 2015 and August 1, 2019. Patient demographics, date of diagnosis, location of main treatment center, and dates and doses of receipt of all BMAs, including ZOL and DEN, were extracted from the electronic medical record. For patients who were switched from one class of BMA to another, we used manual chart review to extract the switch date, reason for switch, estimated glomerular filtration rate (eGFR), and dates and types of all SREs sustained thereafter.
Results:
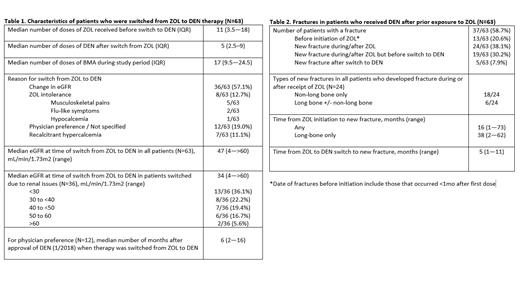
We identified 658 patients who received BMAs for MM during the study period. Among these, 499 (75.8%) received ZOL only, 91 (13.8%) received DEN only, and 68 (10.3%) received ZOL and DEN during their treatment course. Of this last group, 63 were switched from ZOL to DEN. The most common reasons for switching from ZOL to DEN were as follows: change in eGFR (57.1%), physician preference (19%), ZOL intolerance (12.7%), and recalcitrant hypercalcemia (11.1%). Among patients switched due to change in eGFR, the median eGFR at time of switch was 34 mL/min/1.73m2 (range, 4->60). For switches made due to physician preference only, the date of switch was a median of 6 months (range, 2-16) following the FDA approval of DEN for MM indication in 2018. The median number of doses of ZOL (either 4mg, 3.5mg, 3.3mg, or 3mg) received before switch was 11 (IQR, 3.5-18) and the median number of doses of DEN (120mg) received after switch was 5 (2.5-9). Among patients who were switched from ZOL to DEN, 24/63 (38%) developed a new fracture at some time during treatment with either therapy, whereas 5/63 (7.9%) developed a new fracture after the switch to DEN. Time from ZOL initiation to new fracture was 16 months (range, 1-73) for any fracture and 38 months (range, 2-62) for long bone fractures. The median time to a new fracture after switch from ZOL to DEN was 5 months (range, 1-11). None of the patients who were switched from ZOL to DEN due to hypercalcemia developed new fractures during the study period. Out of all patients who received BMAs, 32/658 (4.9%) underwent serum CTX level testing to guide use of therapy.
Conclusions:
After the approval of DEN for MM as an alternative to ZOL, we observed that the most common reasons for switch of ZOL to DEN at our cancer center were due to changes in patient renal function or for bisphosphonate intolerance. The use of serum CTX to guide switch in therapy was uncommon in clinical practice and should be encouraged more. In a selected cohort of patients who were switched from ZOL to DEN, the time to new SRE was shorter than historically reported with DEN only. These data highlight the need for prospective studies on the efficacy of DEN in MM patients who have previously been exposed to ZOL.
Neparidze: Eidos Therapeutics: Membership on an entity's Board of Directors or advisory committees; GlaxoSmithKline: Research Funding; Janssen: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal